You have /5 articles left.
Sign up for a free account or log in.

Penn State University is one of several major public research universities that has provided little information about the statistical models used in its reopening plans.
Patricia McCormick/Contributor via Getty Images
In the middle of August, a group of Pennsylvania State University faculty members posted the fruits of weeks of statistical modeling -- projecting results of their university's plans to bring undergraduates back to State College for in-person fall classes.
They assumed 200 students infected with COVID-19 who were not showing symptoms would arrive on campus, out of a total of 40,000. They assumed the university would receive the results of COVID-19 tests rapidly, within eight hours. They assumed most students would follow social distancing and mask-wearing rules. And they assumed Penn State would test students at roughly the rate the university has announced, counting on it to test 30 percent of those coming to campus before they arrived, and then test 1 percent of faculty, staff and students each day.
Given those conditions, Penn State could expect to use up its quarantine capacity sometime in the middle of the fall semester, the group of professors found.
In this report:
Introduction: A university declines repeated requests to release detailed information on statistical modeling it used to craft plans for the fall, even as a faculty group publishes its own work raising concerns.
Transparency in Decision Making: The question of administrators releasing epidemiological modeling is bigger than any one college or university. It's about transparent decision making.
Modeling and Assumptions: All models rely on assumptions. What assumptions do those modeling COVID-19's spread on a college campus have to make, and do they negate modeling's usefulness?
To Release or Not to Release? Public release of modeling could lead to misinterpretation. But academics say sharing is a key part of improving modeling work.
Requests for Public Records: Inside Higher Ed requested COVID-19 modeling used in decision making from 18 institutions across the country. Only one has provided such documents.
Back-and-Forth at Penn State: As a concerned faculty group asks for more transparency and testing, a university provides few new details and questions their modeling assumptions. The sides appear to disagree on how much contact tracing will help.
‘We’re All in This Together’: A university that has declined to release its COVID-19 modeling threatens to expel students who hold large gatherings -- then asks students who have attended to share details for contact tracing.
“It is then quite possible that thousands of asymptomatic infected students could further spread the disease outside State College upon their return to their homes in Thanksgiving,” a technical paper explaining the modeling said. “The possibility of observing some student death under the PSU plan cannot be discarded.”
That’s to say nothing of the effects on faculty, staff and the local population in the State College area.
But the faculty members suggested a fix: increase testing. Their modeling showed that testing 10 percent of the student population daily would drastically cut the likelihood of students dying, which was already low but not zero. The additional testing would slash the number of students expected to need quarantine rooms and the number of students infected without symptoms. Testing all students before they arrived on campus would have similar effects.
“The intention is to really offer suggestions and positive suggestions and say, ‘Look, you can do this,’” said Sarah Townsend, a Penn State professor of Spanish and Portuguese and organizer for the faculty group, which is called the Coalition for a Just University at Penn State. “It’s not even that expensive, according to their estimates. But it’s absolutely essential to increase the daily surveillance testing and to test everyone immediately. It has really drastic results.”
Timing was tight, Townsend acknowledged. Students were already moving back to campus in the days after the group released its modeling. Penn State’s classes started this Monday. In the last week, Penn State leaders initiated disciplinary actions after several unsanctioned large gatherings of students at fraternities and residence halls.
But concerned faculty members were doing the best they could. The university released its testing plans at the end of July. Faculty groups had been working on different COVID-19 models with what they had.
Penn State didn’t plan enough testing, members of the faculty group worried. Almost as concerning, group members had yet to see evidence from the university’s administration that would justify its reopening and testing plans.
“Over the summer, we consistently asked for information on testing plans,” Townsend said. “We asked for information on what kind of scientific evidence they were using. We asked to see data modeling, other examples, or kinds of evidence that they were using to develop their plans. The university has just been totally silent on that front.”
Asked about the faculty group’s modeling, Penn State’s senior director for news and media relations, Lisa M. Powers, emailed a statement last week.
“This group has advocated against any reopening of campuses,” it said. “This latest, anonymous communication in their advocacy effort fails to properly account for critical factors like contact tracing and adaptive surveillance approaches. The University has been transparent about its plans, which have been developed with faculty scientists, who are health and supply chain experts, to significantly exceed the Pennsylvania governor’s guidance for return to campuses.”
Members of the faculty group disputed several of those characterizations, including that they hadn’t properly accounted for factors like contact tracing in their modeling.
Asked which specific scientists worked on the administration’s modeling and whether it was publicly posted or available, the university’s communications department did not directly respond. Instead, it offered an interview with Dr. Kevin Black, interim dean for the university’s College of Medicine, a professor in the department of orthopedics and rehabilitation, and co-leader of the Health Resources Task Group. That group performed modeling for the administration’s review.
Black declined to name any individuals who performed modeling without first obtaining their individual permission. He also said that he was unaware of anywhere the modeling for the administration had been publicly posted.
“The methodology, I think, is very sound,” he said. “The charge of our committee was to bring recommended options and a contact-tracing strategy to the university. I think it is certainly the prerogative of university leadership to decide what to do with that information.”
Asked again who, specifically, created Penn State’s modeling and whether any documentation had been released, Powers provided additional statements.
“The university’s dynamic model was created by a multi-disciplinary team from our Huck Institutes of the Life Sciences, with a number of researchers from our Center for Infectious Disease Dynamics contributing,” she wrote in one. “We have nothing else to add.”
Informed that the names of the administration’s modelers were being sought because she had initially criticized the faculty group for releasing work anonymously, Powers on Sunday provided four names: Black; Matt Ferrari, an assistant professor of biology and statistics; Dennis Scanlon, distinguished professor of health policy and administration; and Andrew Read, professor of biology and entomology and director of Penn State’s Huck Institute of the Life Sciences.
Ferrari responded Monday to a request for comment by email, saying he led efforts to develop models exploring scenarios for reopening Penn State. He said he was responding on behalf of Scanlon, Read and Black.
The modeling work Ferrari led for the administration approached the issue of reopening differently than that of the independent faculty group, he said. Ferrari’s group modeled testing levels needed to estimate infections on campus and warn officials of increases. It ran simulations showing contact tracing was important -- if you map out all the people an infected person may have interacted with, each positive test is more valuable in the fight to contain COVID-19’s spread in a situation where not everyone is being tested. Ferrari’s group also looked at testing students before they arrived on campus once it was clear infections weren’t dropping across the country.
The Coalition for a Just University, on the other hand, looked at Penn State’s plans and found that frequent testing and isolating infected students were the most important steps to control COVID-19’s spread. Those conclusions were similar to that of research groups elsewhere. Coalition members said that with enough testing, the need for contact tracing diminishes and that many potential pitfalls can be avoided.
Ferrari’s email summarizing the university’s modeling included links to research performed by teams at other universities and an analysis of a past mumps outbreak at Penn State. But it did not document in extensive detail the results of the modeling work the team did for the administration.
Asked for additional reports or documents, Ferrari declined.
“I am sorry that I am not authorized to provide these directly,” he wrote. “For the reports on these analyses I must refer you to the university.”
Transparency in Decision Making
The question of whether administrators will release epidemiological modeling is bigger than any one college or university, and it’s about much more than the modeling itself.
It cuts to the heart of decision making by higher education leaders across the country. How administrators made the decision to reopen campuses for in-person instruction in the fall has been an important point of discussion for months. So too has been what they considered as they crafted plans for testing, reduced density on campuses, mask-wearing requirements and other efforts to combat the transmission of a virus that could easily incubate undetected among groups of young, healthy students concentrated around a college campus -- then leap to older, sicker populations like staff members, faculty members and local residents.
Those considerations are in the limelight after last week, when several prominent research universities pulled the plug on in-person instruction and residence-hall living or locked down campus just a short time after undergraduates arrived earlier this month.
What number of infections were college leaders expecting as campuses opened? How did they decide how many quarantine rooms to set aside? Did they consider how likely it would be that bringing students back to campus could spread COVID-19 infections in the surrounding community and among vulnerable faculty and staff members? Did they consider how many hospitalizations and deaths to expect as a result of their decisions?
And, with many college leaders shaming students for gathering in environments that were designed to facilitate interaction, just what kind of social distancing compliance did administrators expect from 18- to 24-year-olds who were out in the world on their own for the first time in months?
What gets measured gets managed, as the adage goes. College presidents might make one decision if they’re only looking at how much mask wearing cuts transmission rates or the amount of room and board revenue they’ll lose by closing residence halls. They might make an entirely different decision if they’re staring at the number of people they can expect to die as a result of their choices or if they see infection curves that suggest reopening safely will require a bigger investment in testing capacity than they can afford.
Peeking under the hood of any decision-making process is fraught. It’s especially difficult to do in the current pandemic, when uncertainty pervades.
But higher education fancies itself different from other organizations because of its long history of shared governance and its appreciation of scientific evidence. Those things mean subtly different things to different groups, but experts usually agree that transparency serves as a cornerstone of shared governance, no matter who is responsible for specific decisions. Evidence-based decision making is often held up as a way to support courses of action and build trust between different constituencies.
During the pandemic, modeling provides a unique opportunity for transparency in evidence-based decision making. That’s because explaining modeling can force leaders to lay out the factors behind the decisions they reach, as well as they assumptions they’re forced to make.
It’s possible to make good decisions without conducting statistical or epidemiological modeling. Some institutions did not have the resources to do such work themselves. But in a pandemic situation, it is fair to ask leaders at major research universities with public health expertise on their campuses how they knew what to expect before they returned undergraduates to classrooms.
“It would be grossly irresponsible for any school to reopen without running the numbers and generating expected and worst-case scenario estimates of things like quarantine space, severe symptoms and deaths,” Doug Webber, an associate professor in the Department of Economics and Institute for Labor Economics at Temple University, said in an email.
Academics who work with statistical models are quick to stress that they can’t predict the future. Any modeling is a simplification of reality that can miss important variables. All relies on assumptions.
Those who’ve modeled COVID-19 infections on campus have to make assumptions like how contagious the virus will be, how effective testing will be, the percentage of infected people who won’t experience symptoms and, depending on what they’re examining, the likelihood that different groups of people will experience complications.
Generally, modelers’ strategy is to scan research for the best available information to help them make those assumptions. But they acknowledge reality will unfold differently than the simulations they run, no matter how hard they work to feed good data into their models.
When interviewed, modelers frequently bring up a common saying in statistics: all models are wrong, but some are useful.
In the case of colleges reopening campuses, this means that modeling could allow leaders to know with some degree of confidence what to expect this fall. It can also help them understand how to change their strategies to give them the best chance of preventing a dangerous escalating outbreak that could push local hospitals beyond capacity.
“We can see: What are the things that are the riskiest parts of the strategy?” said Nigel Goldenfeld, a professor in physics at the University of Illinois at Urbana-Champaign, during an online presentation earlier this month on COVID-19 modeling that the university used in making its fall reopening plans. “Our work has already led to two different changes. One is we are testing twice a week.”
Models can also be used to make an argument. That’s what Joshua S. Weitz, a professor of biological sciences at Georgia Tech and founding director of the quantitative biosciences Ph.D. program there, did last month. He presented findings to an academic restart committee showing what would happen if the university didn’t mitigate the virus’s spread on campus. If campus had reopened at full capacity and half of everyone became infected, Georgia Tech could expect about 75 fatalities, he found.
For college and university leaders who have to make decisions, models can have a huge upside.
“You would think or hope that institutional leaders, when making decisions on fall enrollment and fall reopening plans, would bring to bear some sort of epidemiological model that would give them a sense of what the infection rate might look like under different scenarios,” said Kevin McCarthy, senior consultant for the Association of Governing Boards of Universities and Colleges.
With good data around which to build assumptions, statistical modeling could be useful in making reopening plans, said McCarthy, who stressed he is an education analyst and researcher but not an epidemiologist. At the same time, he could see why some leaders might not have relied on statistical models.
“As you add more assumptions to each of the inputs, you increase the inherent uncertainty of the outcome,” he said. “I can imagine university leaders looked at the landscape of possibilities when making fall reopening plans, and they probably saw that building a model was going to be time-consuming and in some cases difficult. And we wouldn’t have any expectation that the output would be terribly useful in understanding what impact our decisions might have.”
Yet several university leaders have said in recent weeks that they used modeling in crafting their reopening plans.
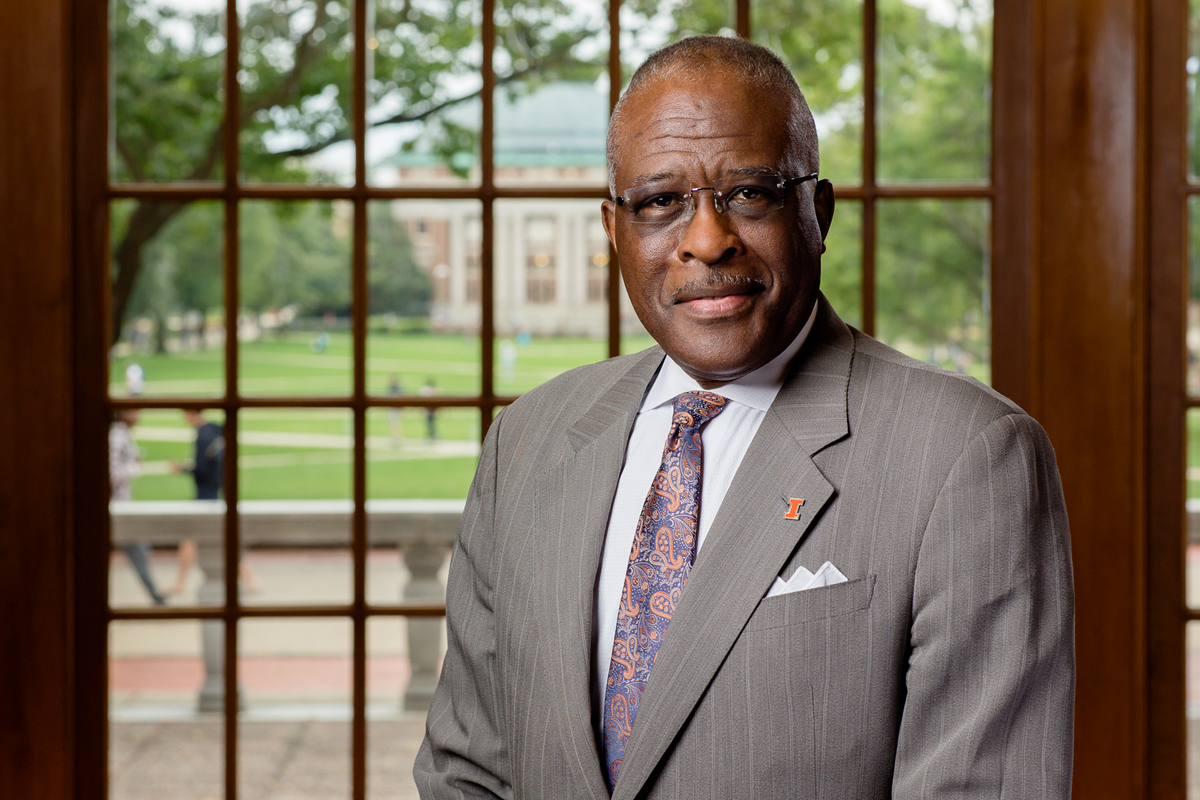 Among them is Robert Jones, chancellor of the University of Illinois at Urbana-Champaign. Experts’ modeling work gave university leaders confidence when planning, he said in a Friday conference call with reporters.
Among them is Robert Jones, chancellor of the University of Illinois at Urbana-Champaign. Experts’ modeling work gave university leaders confidence when planning, he said in a Friday conference call with reporters.
“The question we are hearing is this: What makes you think you can open the semester with in-person classes?” Jones said. “Well, it’s because we have our own innovative new saliva-based test, data-driven modeling for our processes and our infrastructure to deploy our testing with the frequency and the scale that we have put into place.”
Because of the models they ran, leaders at Illinois were bracing for a wave of infections after students started moving in Monday.
“We know we’re going to get a bump, and we’re really looking forward to the fast and frequent testing,” Martin Burke, associate dean for research at the university’s college of medicine and chair of a COVID-19 team there, said during the call. He emphasized the message that everyone will need to be extra careful for several weeks following move-in, even as others on the call stressed that frequent testing is key to their strategy.
“We know we have to test, but what is the best way to deploy it?” Goldenfeld, who also is helping the state of Illinois with modeling, said Friday. “We discovered we have to do it twice a week in order for it to be as effective as we wanted it to be. Other studies also confirmed that later and independently.”
Michigan State University’s president, Dr. Samuel L. Stanley, called off plans to bring undergraduates back for in-person classes last week, just days before students were scheduled to start moving in. Several sources of information led to that decision, including the experience of other universities that had experienced cases surging, he said.
When Michigan State made its reopening plans, it used statistical modeling, Stanley added. It focused on surveillance testing. It also examined hospital capacity in case of outbreaks.
“It’s very nice to have empiric evidence in front of you,” Stanley said in a call with reporters.
Those administrators that did use modeling in their decision making must decide how to communicate about it, as well as what kind of information to release.
Some avoid releasing models. Knowledge about the virus -- and the data to feed into models -- is constantly changing.
Results could be easily misinterpreted. An early model or one that used inaccurate assumptions could lead to public misunderstanding. Public release of explosive projections such as likely deaths could lead to fearmongering.
Plus, administrators don’t usually like to give the public cause to second-guess their decisions.
“I'm betting that most schools have done at least some rudimentary modeling of this, and I also bet it was done via outside consultants rather than internal researchers,” said Webber, the Temple professor. “If you do it via an outside firm, you have to pay more for it, but you can control what gets released. If a university uses their own faculty, who are protected by academic freedom, there is a very good chance that these numbers would get out to the public.”
Still, those who have worked with statistics say that public release of modeling is a best practice. It allows for others to examine assumptions and improve the work.
It is, in other words, a way to allow for peer review and to follow an iterative scientific process -- concepts at the heart of modern scholarship.
Cornell University’s president, Martha Pollack, cited modeling earlier this summer when announcing fall plans including in-person instruction. At the time, the modeling found an in-person semester was likely safer than one online. A core part of that determination was an assumption that about 9,000 Cornell students would return to live in Ithaca, N.Y., regardless of whether in-person learning resumed in the fall. The university would be able to test off-campus students if they held in-person classes, and testing is key in containing COVID-19.
Researchers involved in the Cornell modeling have been taking comments on their work on a public website. They’ve also updated it to account for changes since their initial findings: increasing infections in parts of the United States, the potential for Cornell students to lack access to testing at home and a new requirement that people traveling to New York State from areas with high levels of infection must self-quarantine when they arrive, no matter what testing shows.
Researchers built a model for Emory University in Atlanta that has been published as a preprint paper, meaning it has yet to be certified by peer review. They also posted an interface online allowing anyone to change key conditions in hopes that the model could be helpful for other colleges and universities. The effect is that members of the public can change key variables and assumptions for themselves to better understand how the model works.
“While we present numerical results for our university at a specific point in time, the model can be reparameterized for other institutions and can be updated as the epidemiological situation shifts,” the researchers wrote in the preprint paper. “We updated the model a number of times in discussions with our university leadership. Results from this framework have been influential in their ongoing decision-making.”
Emory brought select students -- including first-year students, international students, some seniors completing honors work and students with special housing needs -- back to campus from Aug. 13 through Aug. 17. About 1,600 students were expected to live on its Atlanta campus, down from about 4,400 last year. Occupancy was limited to one student per room.
Others have been trying to provide modeling resources for institutions that may not have expertise in-house or the money to pay for extensive statistical work. A group of faculty members and undergraduates at Baruch College, Grinnell College, Bard College and Cornell University recently released a preprint copy of modeling that simulates students and faculty members moving onto a campus with about 2,000 students.
They found most people would become infected within a few months without interventions or mitigation strategies. A combination of testing, quarantining, mask wearing and reduced student density made a big difference, though.
“There are real decisions that college administrators, personnel and students can make going forward that would actually make it more viable for them to be in residence on campus,” said Felicia Keesing, a biology professor at Bard College and co-author of the study. “What we found is that having a pretty high frequency of screening tests and a very quick turnaround in test results made a huge difference.”
Strict policies and students adhering to those policies are also important, according to the team’s work.
Students on the team helped researchers understand how certain decisions could affect on-campus behavior in ways that older adults might not expect. For example, researchers modeled what would happen if an institution closed a dining hall, because many colleges and universities have decided to do that, Keesing said. Students told them they were making a hidden -- and likely incorrect -- assumption: that if you close the dining hall, students will go to their dorm rooms and eat by themselves.
“Students will congregate,” Keesing said. “They will just congregate elsewhere.”
Having that perspective didn’t eliminate all uncertainty. Researchers still had to make an educated guess about how many students would congregate in such situations. But the process had exposed them to a new way of thinking and a new set of considerations.
It’s also important to remember the limits of a model, Keesing said. The model she worked on didn’t include staff members, because it was more than could be crammed into the work in the time the team had available. Staff members work such a wide variety of jobs that modeling their behavior or risk of catching and transmitting the virus is exceptionally complex.
That doesn’t mean potential effects on staff members should be ignored.
“You can come away saying, for example, that closing the dining hall could be worse because you end up with more student infections,” Keesing said. “But one of the arguments for closing the dining hall is actually to reduce staff vulnerability.”
Without listening to others about the limits of the model -- the limits of their own thought process -- the team might not know what it was missing.
“Transparency is the whole point,” Keesing said. “That’s how science is supposed to work. That’s why we post our code, so you can look through the code.”
College and university leaders across the country have explained their decision-making processes for the fall at this point. Often, they’ve done so by pointing to a dense web of workgroups and subcommittees tasked with looking at the question of reopening from multiple angles. But some have been willing to share more than others.
In an attempt to better understand higher education leaders’ decision-making processes, Inside Higher Ed submitted public records requests to 18 different state institutions at the end of June. The requests sought contingency plans, scenario planning, risk assessments and other plans modeling potential COVID-19 infections, hospitalizations and fatalities related to holding in-person instruction or reopening campus for the fall 2020 semester.
Fourteen of those institutions had issued final responses to the requests by the end of last week. Just one, Georgia Tech, provided documents detailing modeling that had been presented to a faculty reopening committee.
It is possible that the wording of the public records request did not cover certain modeling or other documents that do in fact exist. Wording any public records request is a delicate balance between being wide-reaching and being specific. Requests need to be expansive enough to return a range of documents that provide insight into leaders’ thinking. They need to be specific enough that colleges and universities do not reject them for being overly broad.
Penn State, which is exempt from Pennsylvania’s public records law, was not among those institutions queried. The results of the project reveal that Penn State is far from alone in not releasing detailed statistical modeling its leaders may have used.
West Virginia University found no documents that were responsive to the request, according to an email from its Freedom of Information Act office.
“Further, even if the WVFOIA request was more specific, unpublished or draft COVID-19 contingency, scenario or assessment planning documents and models are exempt from public disclosure as deliberative drafts and risk assessments of the University,” the response continued.
Inside Higher Ed contacted college and university communications offices in cases where no documents were returned. In many cases, officials responded by providing an overview of their fall plans or links to websites detailing how colleges would reopen. Some did not address a specific question about whether any modeling was conducted.
“I can confirm that no records met the description you sent in,” wrote Leslie Minton, associate director of media relations at the University of North Carolina at Chapel Hill, in an Aug. 12 email, also providing a link to the university’s “Roadmap for Fall 2020” website. That website included details about efforts to mitigate on-campus viral spread but appeared to have few, if any, details about how the university developed them -- save for a set of guiding principles that included a bullet about relying on public health experts and using “evidence and science to monitor our strategies and develop interventions as needed.”
Asked for additional comment, including answers to yes or no questions about whether Chapel Hill had evaluated any projections to determine the number of staff, students or faculty COVID-19 infections to expect, Minton sent another statement.
“Carolina has taken a thorough and holistic approach to planning for the fall semester that incorporates a number of important data points and is reflected in our Carolina Together website. Beyond that, we have no further information to share about projections,” Minton wrote on Aug. 13. “The University also is continually monitoring the above data points and will work in consultation with the UNC System and local health officials on operational decisions.”
Chapel Hill brought undergraduates back early this August. Last Monday, a week after classes started, the university announced it was sending undergraduates home amid a spike in infections and dwindling rooms reserved for quarantining. Its testing positivity rate rose from 2.8 percent to 13.6 percent in a week.
Friday, Chapel Hill’s student newspaper, The Daily Tar Heel, ran an article based on its own public records request. In part, it reported that the president of the UNC Health Foundation emailed the university’s vice chancellor for university development May 15 with models showing hospitalizations through the end of the year.
Asked about this development, Minton again did not address any modeling the Chapel Hill administration may have used.
“To clarify, UNC Health is a separate entity from the University. I recommend you reach out to their team with any questions on UNC Health public records,” Minton wrote in an email.
The president of the UNC system issued a statement last week on Thursday, when another of its institutions, North Carolina State University, said it was moving exclusively to online classes amid its own coronavirus outbreak.
 “Over the spring and summer every institution prepared for the fall semester under the guidance of well-known public health officials,” said the system president, Peter Hans. “The planning reflected the fact that each university in the system is different -- with diverse student populations, geographical locations and varied social cultures. This hard work is being undermined by a very small number of students behaving irresponsibly off campus, which unfairly punishes the vast majority of their classmates who are following the rules.”
“Over the spring and summer every institution prepared for the fall semester under the guidance of well-known public health officials,” said the system president, Peter Hans. “The planning reflected the fact that each university in the system is different -- with diverse student populations, geographical locations and varied social cultures. This hard work is being undermined by a very small number of students behaving irresponsibly off campus, which unfairly punishes the vast majority of their classmates who are following the rules.”
Another institution in the system, East Carolina University, last weekend announced it is suspending classes and will start holding them online. The university, which started classes Aug. 10, will begin moving students out of residence halls this week. It counted 125 cases among students and staff.
Michigan State and Illinois were among universities that did not return modeling documents in response to Inside Higher Ed’s request. A Michigan State spokeswoman said the university’s modeling did not generate documents that the public records request would return. An Illinois spokeswoman said the university had interpreted the request to be focused on reopening plans and not models used in decision making.
Both of those universities made leaders available or were responsive to follow-up questions.
Several other institutions are still processing requests. Others provided links to forward-looking documents or other planning documents that do not detail any statistical modeling.
One trend that emerged is that, in contrast to some flagship institutions, less wealthy and less prominent universities were open about the fact that they did not conduct modeling themselves.
Three community colleges queried were among the most responsive institutions. Tulsa Community College provided hundreds of pages of emails that showed administrators monitoring local infection counts, among other discussions. But it did not provide any modeling.
“Tulsa Community College administration did not do any of its own modeling,” Nicole Burgin, media relations manager for the college, said in an email. “We are a community college and not a research university. In addition, we do not have on-campus housing nor athletics. However, we relied on heavily the expertise and guidance of the Tulsa Health Department, Oklahoma State Department of Health and the Centers for Disease Control and Prevention to shape our Return to Campus plan.”
The community college lists fall classes as resuming with online, blended and face-to-face class option. Two other community colleges provided similar responses.
“We are a commuter institution and I can see how some institutions with housing and students on campus 24/7 have used modeling,” said Juan Mendieta, communications director at Miami Dade College, in an email. “The only modeling we have used related to COVID is for classroom and space utilization to determine the campus footprint for classes should we resume classes on campus with social distancing and reduced room capacities in place.”
A spokesperson for Grand Rapids Community College provided a copy of its preparedness and response plan, along with a brief description of the risk categories for different groups on campus.
Miami Dade plans to start fall classes by remote learning, with a return to campus coming no earlier than Sept. 14. Grand Rapids plans fall classes including expanded virtual offerings, hybrid classes and on-campus classes.
“Grand Rapids Community College worked with a template created by the Michigan Department of Labor and Economic Opportunity and the Michigan Department of Occupational Safety and Health Administration. This plan includes an exposure determination,” Dave Murray, communications director at Grand Rapids Community College, said in a statement. “As part of this process we have worked closely with the Kent County Health Department as well as state and federal agencies for guidance on developing robust health and wellness protocols moving into the fall semester.”
The University of Houston also was clear that it did not model projections for infections or hospitalizations specific to its campus. A spokesperson there said the university looked at a number of different factors to prepare and plan for the fall, including projections from the Texas Medical Center, state guidance, faculty and student course delivery preferences, facility capacity allowing for social distancing, and protocols to respond to positive cases on campus.
“The university did not model projections of COVID-19 infections or hospitalizations specific to UH,” Shawn Lindsey, executive director of media relations, said in an email. The university recently moved in students, with classes beginning on Monday this week, including face-to-face, HyFlex and online offerings -- although Hurricane Laura prompted it to move instruction online.
The State University of New York’s Binghamton University, which brands itself as “the best public university in the Northeast,” pointed to two public-facing websites outlining fall plans. Neither of them detailed epidemiological modeling.
Asked about modeling specifically, a spokesman said the university worked with public health experts.
“Binghamton also worked directly with two regional health care providers (hospital systems) through a county emergency operations group to model the return of students to the local community,” the spokesman, Ryan Yarosh, said in an email. “The campus provided ZIP code and other de-identified data for our student population from which analysts from the hospital systems evaluated the potential impact on hospital bed demand and infection rates. While this data is ever-changing, the very low infection rates in almost all New York regions from which our student population will arrive suggests that the return of our students can be achieved safely.”
Yarosh added that an analysis by Upstate Medical University’s public health department pegged the risk of students returning to Binghamton’s campus as “very low to low.” The university expected on-campus occupancy to be about 85 percent of normal.
Institutions with fewer resources being less likely to do their own modeling is to be expected, according to leadership experts.
“The models are complex,” said McCarthy, the senior consultant at AGB. “They require a lot of inputs and a lot of assumptions. Unless you are a large, R-1 research institution with an affiliated hospital or a big public health program, you probably don’t have the data or access to the experts who can get the data just lying around.”
Depending on your perspective, that could be an argument for learning to do planning in uncertain situations without expertise-intensive statistical modeling. Or it could be an argument for those that can do the modeling to release their findings so that others can learn from it.
Where does this discussion leave a campus with faculty members who feel administrators haven’t been forthcoming, but where the administrators aren’t budging -- a campus like Penn State?
The Penn State example is complicated because little trust exists between concerned faculty members and administrators. The faculty group posting its modeling about COVID-19 infections wrote an open letter to the university administration two months ago voicing concerns about plans for the fall semester.
Those concerns included that faculty members had been given limited input into decisions about safety, job security and method of instructional delivery. More than 1,100 faculty members signed it, along with almost 500 graduate students, undergraduates, staff members and others.
The group continued to push for information from the administration and didn’t receive anything satisfactory, according to Townsend, its organizer.
“We have no idea what information they’re using to develop their plans,” she said.
Ferrari, the assistant professor of biology and statistics who led group modeling efforts for Penn State’s administration, has provided perhaps the most detailed discussion of the statistical work the administration reviewed -- in the email he sent Monday.
“We modeled outcomes such as the proportion of asymptomatic tests that were positive, the daily number of symptomatic cases and daily hospitalization rates that could be used [as] indicators of the need for changes in University operations,” Ferrari said via email. “We developed simulations to illustrate the importance of a robust contact tracing system to supplement asymptomatic and symptomatic testing.”
Contact tracing and finding additional cases mean that each positive COVID-19 test has additional benefits, Ferrari wrote. His group’s work for the Penn State administration showed that investment in contact tracing, isolation and quarantine facilities were needed to realize the benefit of a “less than universal” testing strategy.
Ferrari’s group considered the way COVID-19 counts across the country could affect outcomes, he said. When national virus prevalence didn’t fall over the summer, the group considered pre-arrival testing as a way to cut the number of infected students arriving on campus. That formed the foundation for the pre-arrival testing strategy Penn State put in place.
“A large group of faculty from across the university worked to develop a range of scenarios and assess their operational feasibility, given scale and supply chain limitations,” Ferrari wrote. “These were presented to the administration for their consideration in the formulation of their operational plan.”
Black, the interim dean for the university’s College of Medicine who was also involved in modeling work used by the Penn State administration, stressed that plans may change based on evolving conditions.
“Our thought process included taking into consideration the need to do prevalence testing in a relatively short time frame, pre-arrival testing prior to the students returning to campus, but also recognizing that the surveillance testing that we’re thinking about after the students arrived might need to be modified,” he said.
Penn State officials have also pointed to a July 30 virtual town hall event as evidence they shared details about their planning. During that town hall, Black said the university's testing strategy was designed to provide multiple options and "mitigate the risk associated with decreases in capacity for any one approach or any one vendor."
Members of the concerned faculty group at Penn State, the Coalition for a Just University, said it was reassuring to hear Ferrari’s description of “serious modeling undertaken by expert faculty.” But they said they’re still troubled that the administration hasn’t released more details about the modeling or its projections. They’ve released details about their modeling. Why, they asked, couldn’t the university do the same?
“What they’re asking is for us to have faith,” said one of the professors who was on the group's modeling team but who would only speak on a condition of anonymity because of fears of retribution from the administration. “In an academic institution, you cannot act like that. We are scientists. We would like to see evidence.”
Penn State officials have blasted the independent faculty group for not taking into account contact tracing, among other parts of the university’s plans. One statement from Powers, the university’s senior director for news and media relations, said that “the model put forward by these anonymous individuals does not include many of these factors and, hence, is flawed. We will continue to keep the community informed of the University’s health and safety efforts through this difficult time.”
The group of concerned faculty members pushed back strongly on these criticisms. The technical documentation the faculty group released explicitly states that their modeling used a low virus reproduction number, which in part approximates “the effect of contact tracing, masks, social distancing while on campus, etc.”
Coalition members stressed that they evaluated the testing plans Penn State has released, including the level of contact tracing expected. They also looked at alternatives such as testing more frequently during the semester and when students arrived on campus.
They found that with enough testing, the need for contact tracing and isolation drops dramatically. The test-and-trace approach Penn State is following will not reduce the reproduction rate of the virus enough to stop the virus from spreading, they said, citing a recent study from the academic journal The Lancet.
That type of back-and-forth is far from unheard-of in charged scientific discussions. In the worst cases, it can lead to gridlock and members of the public -- who aren’t experts able to evaluate certain complex arguments and assumptions -- throwing up their hands in confusion.
Think about the issue of global climate change, where the fossil fuel industry for years refuted scientific models by quibbling with assumptions or releasing its own work. Still, widespread agreement exists among scientists that humans releasing carbon dioxide into the atmosphere is driving up temperatures around the world.
”You can focus on those predictions if you like those predictions, and if you don’t like those predictions, you can point to the assumptions to undermine the model,” said Keesing, the biology professor at Bard College who co-authored a study modeling movement on a campus of 2,000 students. She was speaking generally about statistical modeling and transparency, not about the Penn State situation.
“All you have to do is challenge the assumptions of those models,” she said. “And we’re at loggerheads.”
In recent weeks, college and university leaders across the country have punished students for risky behavior and issued stern warnings that more is to come for those who don’t follow the rules.
That’s prompted concern among some adolescent behavior experts and epidemiologists. They worry crackdowns don’t deter risky behavior but instead tend to drive it out of sight.
Even leaders of campuses that aren’t holding in-person classes this fall struggle with a balance between deterrence and fostering a climate of trust.
Carol Christ is the chancellor of the University of California, Berkeley, which announced in June it would be starting the fall with fully remote instruction. Berkeley officials expect about 1,700 students to live in university residence halls, down from a normal capacity of 9,600 because of social distancing measures and students canceling their housing contracts.
“What we don’t want to do is make students fearful of punishment so they don’t want to get tested or they hide -- either the illness or behavior -- in some way or another,” Christ said in an interview Monday about Berkeley’s fall plans. “I think it’s a very complex balance between the, if you like, the iron fist and the velvet glove.”
The right balance may be different depending on a university’s strategies for combating the pandemic -- whether it relies more on reduced density on campus, frequent testing, openly sharing information or contact tracing.
Again, consider Penn State.
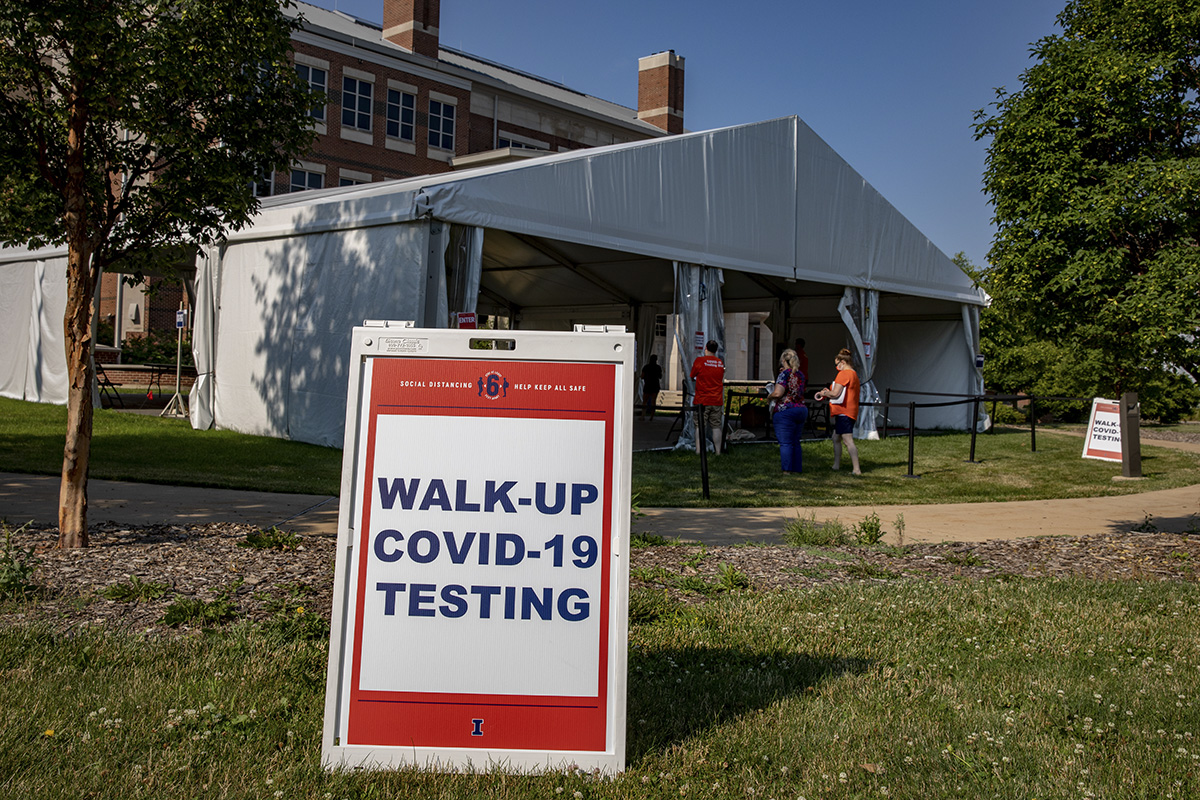 Penn State plans to each day randomly test about 1 percent of students, faculty and staff on campus, adjusting that number as necessary. That means for now, everyone could be expected to be tested once every 100 days. For comparison, the University of Illinois at Urbana-Champaign plans to test everyone twice a week.
Penn State plans to each day randomly test about 1 percent of students, faculty and staff on campus, adjusting that number as necessary. That means for now, everyone could be expected to be tested once every 100 days. For comparison, the University of Illinois at Urbana-Champaign plans to test everyone twice a week.
A COVID-19 dashboard at Penn State will be updated weekly. It shares data like the number of tests performed and tests returned positive for students and employees.
That dashboard does not include results from individuals who were tested before arriving on campus. Penn State’s surveillance testing began Monday, so the dashboard contains a disclaimer that data will be limited for the first week until tests are returned.
More transparency is needed, according to members of the Coalition for a Just University at Penn State. They pointed out that Ferrari, who led the modeling that fed into the university’s fall planning, said his group drew upon an analysis of a 2017 mumps outbreak at Penn State.
“To effectively manage transmissible pathogens, students must cooperate with university outbreak management efforts and comply with behavioral interventions. Universities must provide timely, transparent outbreak updates, develop clear guidelines for action and reward compliance in contact tracing, quarantine and isolation protocols,” that analysis concluded. “Student compliance with behavioral interventions and contact tracing can save lives. Universities must emphasize the health benefits to individual students and the community.”
Penn State’s administration has released a series of statements condemning students for unsanctioned large public gatherings -- while also revealing that administrators suddenly need students to come forward.
Last week came a statement from the university’s president, Eric Barron, condemning reports of “crowds of students congregating in large numbers outside of East Halls on the University Park campus,” many without masks or practicing physical distancing.
 “Last night’s behavior is unacceptable,” Barron said. “I ask students flouting the University’s health and safety expectations a simple question: Do you want to be the person responsible for sending everyone home?”
“Last night’s behavior is unacceptable,” Barron said. “I ask students flouting the University’s health and safety expectations a simple question: Do you want to be the person responsible for sending everyone home?”
The same day, the university announced that its Phi Kappa Psi fraternity chapter was placed on interim suspension in response to an Aug. 18 gathering where “photos and videos shared on social media depicted more than 15 individuals gathered indoors not wearing face coverings or participating in physical distancing.” The gatherings were in violation of various university requirements designed to slow or stop the virus’s spread.
Sunday brought news that the university suspended another fraternity chapter, Pi Kappa Alpha, for a large gathering the day before with about 70 students in attendance. The gathering included at least 36 who weren’t residents of the fraternity house in question. Penn State suspended fraternity chapter executives who didn't obey university monitors.
“Social gatherings are among the very best ways to spread the virus, and refusing to comply with the public health mandates, even when directed to do so by University officials, will not be tolerated,” Penn State’s vice president for student affairs, Damon Sims, said in a statement.
Penn State was requiring fraternity members to be tested for COVID-19. The university was also encouraging students who weren’t Pi Kappa Alpha members but who might have attended Saturday’s gathering to be tested. Likewise, it urged students who gathered at East Halls to be tested -- acknowledging that it had yet to identify them.
No disciplinary action would be taken against such unidentified students who showed up to be tested, the university promised. Its goal is to rule out possible coronavirus exposure.
"We're all in this together, so when one of us, or a group, behaves in ways that threaten all of us, we must act, and we must act quickly," Sims said.
Greta Anderson, Lilah Burke, Lindsay McKenzie and Madeline St. Amour contributed reporting to this article.