You have /5 articles left.
Sign up for a free account or log in.

John Freyer and his “free naloxone bike” on the Virginia Commonwealth University campus. More colleges are taking innovative approaches to make the overdose-reversing drug accessible to students.
Photo by Enza Marcy
Students at Virginia Commonwealth University might run across a new but familiar sight while walking through the Richmond campus this fall: a man on an electric bicycle, the words “free naloxone bike” laser-etched into a wooden lockbox above the handlebars.
That man would be John Freyer, an associate professor of cross-disciplinary media at VCU. He’s been biking for a cause on campus since 2016, when he started a “free hot coffee bike” project where he and student volunteers dispensed mugs of freshly brewed joe along with conversation about substance use stigma, addiction recovery and harm reduction.
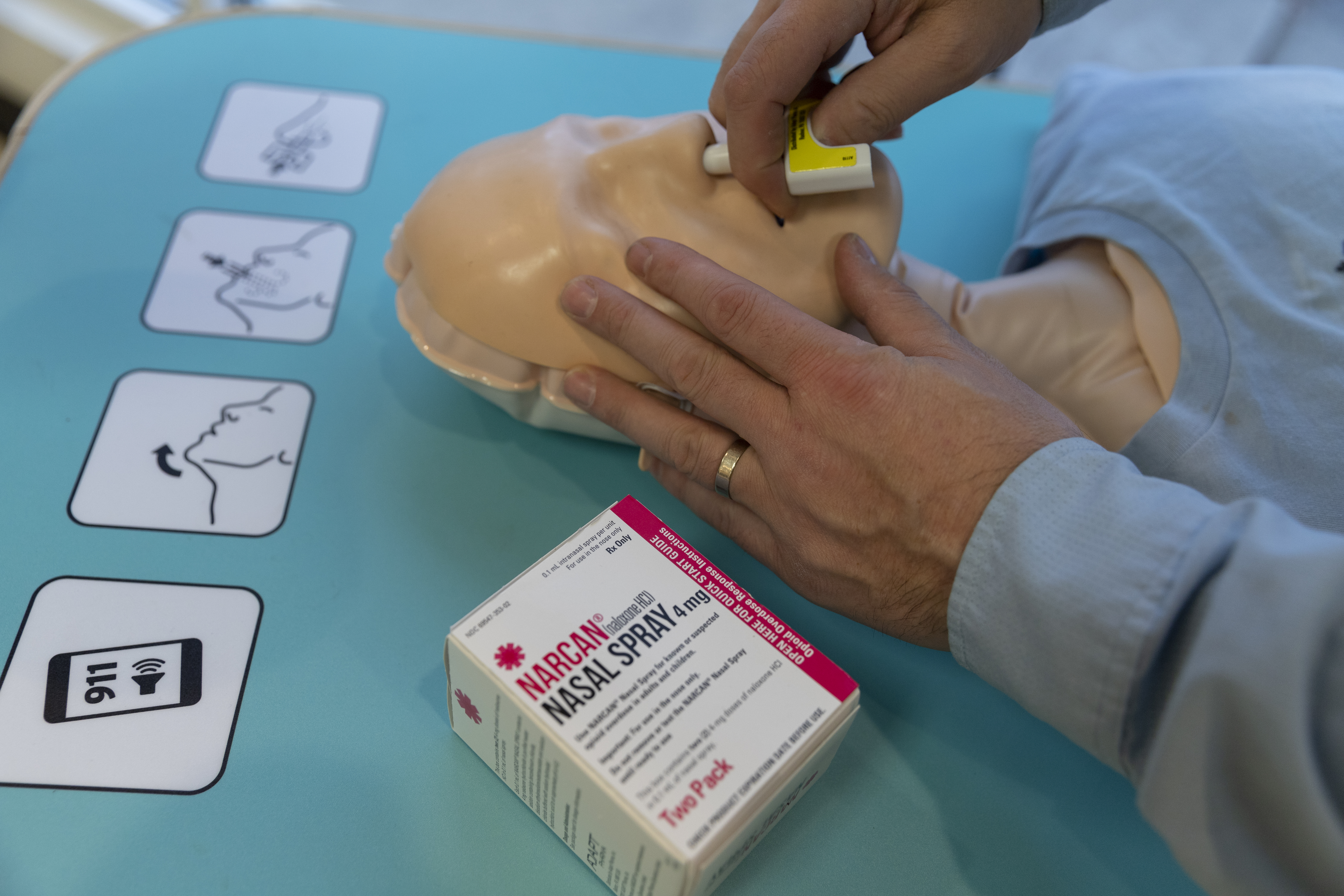
Freyer, inspired by the project’s success, launched the free naloxone bike as a kind of spinoff in February 2020. Instead of coffee and brewing gear, the new bike is equipped with a wooden box that can hold up to 100 doses of naloxone, an emergency medication that reverses the effects of an opioid overdose; a practice dummy named Mannie Fresh rides in the back seat. Interested students and community members with a few minutes to spare can get trained and go back to their dorm or apartment with the knowledge and tools they’d need to save someone who was experiencing an opioid overdose.
Because naloxone is a schedule IV drug under Virginia law, VCU would have to become a licensed naloxone distribution site to hand the medicine out to students. Freyer said that universities might understandably be hesitant to take on this designation, so he got his bikes legally designated as distribution sites instead.
“Universities don’t necessarily want to be distribution sites for NARCAN,” Freyer said, referencing the brand name for a nasally administered version of naloxone. “That’s one way the bike helps."
Overdose prevention and substance use education are personal issues for Freyer. He got sober shortly before accepting his current job at VCU and said that working to help others on campus with substance use disorders and to prevent overdose deaths has been an important part of his recovery journey. The pandemic interrupted plans to make the free naloxone bike a fixture on the Richmond campus, but Freyer says it will be out and about making regular rounds next semester.
It’s an innovative approach to a growing trend at colleges and universities: making naloxone widely accessible across campus, and training as many students as possible to use it.
Opioid use is fairly low among college students as a whole—according to a 2021 survey by the American College Health Association, only 0.5 percent of student respondents reported using heroin or prescription opioids recreationally. But the risks of overdosing have increased as the opioid epidemic has worsened: a 2017 study from Columbia University psychiatry professor Patrice Malone found that opioid use among college students is often underreported, and that nonmedical use of prescription opiates is the second most common form of drug use among college students in the United States.
One of the major causes of campus opioid deaths isn’t even purposeful ingestion of opiates. In recent years popular campus drugs like cocaine, Xanax and Adderall have become risks for opioid overdose, as lethal traces of the synthetic opioid fentanyl creep into the U.S. supply. Two Ohio State University students overdosed in May after taking fake Adderall pills.
 “What that context does is it changes the range of people who are at risk for an opioid overdose, and changes it at a very fast rate,” said Max Moss, a Yale University medical student who founded a student-led naloxone distribution and training program while he was an undergraduate at Stanford University. “Even students who don’t think of themselves as drug users but might buy Adderall to help with their academics. They’re also at risk now.”
“What that context does is it changes the range of people who are at risk for an opioid overdose, and changes it at a very fast rate,” said Max Moss, a Yale University medical student who founded a student-led naloxone distribution and training program while he was an undergraduate at Stanford University. “Even students who don’t think of themselves as drug users but might buy Adderall to help with their academics. They’re also at risk now.”
Freyer said he’s working to expand the free naloxone bike model to as many universities as are interested. Programs at Georgia Tech, Virginia Tech and Teesside University in Britain have already adopted the free hot coffee bike, and in June VCU hosted the national conference for the Association of Recovery in Higher Education, where Freyer demonstrated the naloxone bike to over a hundred colleges. Stanford University’s campus recovery program is planning on launching its own as soon as it can secure funding.
“My ambition is to have a fleet of them,” he said.
From the Clinic to the Dorm Room
On most college campuses, if a student wants a naloxone kit, they have to go to their campus health clinic, a local pharmacy or the campus police. But harm-reduction advocates say the ideal strategy is to make the lifesaving medicine easily accessible to as many people as possible, whether those are resident assistants, faculty members or students who want to be prepared.
In 2017, Bridgewater State University in Massachusetts became the first university in the U.S. to keep a publicly available supply of naloxone kits stashed around campus after a student died of an overdose the year before. Other institutions, like the University of Texas at Austin and Ithaca College, followed suit.
Lisa Miller, who was responsible for Colorado State University’s drug and alcohol treatment programs for two decades before her retirement in June, said she became interested in making NARCAN accessible to students after hearing about fentanyl-laced drugs on campuses. She experimented with providing the medicine in the university counseling office and said student interest was apparent.
“The first time I put NARCAN in our waiting area, within 30 seconds, three students picked up a box,” she said. “None of them recreationally used drugs, but they were aware of the problem with the opioid crisis and fentanyl and wanted to be equipped.”
Miller and others at CSU worked on implementing a NARCAN training and distribution program for resident assistants in 2018, but they faced some pushback. After working to develop a fully-fledged opioid education curriculum, the university is launching a campuswide naloxone distribution and overdose prevention program in the fall.
“I think people were afraid of it at the beginning, and universities always have to manage messaging,” Miller said. “But my experience is that if you educate the public they’re right with you. We’re starting to hear parents say, ‘We really support this—how can we sign our kid up?’”
Jennifer Plumb, the founder of the naloxone training and opioid education nonprofit Utah Naloxone, said colleges administrators' consternation about making NARCAN widely available can be chalked up to two main factors: public relations hand-wringing and a sense of denial that students might need the medicine. She says that’s starting to change.
“It’s like colleges thought that by putting naloxone in places on campus they were saying, ‘We have a problem,’” said Plumb, who is also a professor of pediatrics at the University of Utah. “But I’ve definitely seen more colleges reaching out and being much more broad in their approach … I feel like there’s absolutely more acceptance.”
Plumb said that while she believes the recent trend of media stories about fentanyl-laced marijuana or lethal doses on dollar bills is largely sensational, it has had a positive side effect: concerned parents are putting pressure on universities to make NARCAN more accessible.
“I think that parents getting ready to send their kids off are certainly influenced by what they see in the media or read on social networks,” she said. “For the first time in my career, I’ve had moms reach out to me talking about sending their kids away to school with naloxone.”
“It’s just a different world that we live in even than two or three years ago, with the tainted drug supply that we’re seeing,” said Noel Vest, a postdoctoral fellow at Stanford specializing in substance use disorders and recovery. “With that changing world, you need a change in approach.”
Public Health Partnerships
Some states are recognizing college campuses as important battlegrounds in their fight against the opioid epidemic.
In California, where three suspected student overdose deaths at the University of Southern California in 2019 prompted calls for overdose-prevention resources, a newly proposed bill would set aside $50 million to educate state youth and adolescents about the risks of opioids and require all California State University system campuses and state community colleges to make naloxone kits and overdose education available to students. In Washington State, where three Washington State University students died of opioid overdoses in 2016, all colleges that accept state funding are required to develop plans to stock residence halls housing more than 100 students with naloxone kits.
In January 2020, Pennsylvania’s governor, Thomas Wolf, announced that the state would award $1 million in federal grants to higher education institutions for the purpose of creating and bolstering naloxone distribution and training programs.
One of the recipients was a student-led organization called End Overdose Together, which received $100,000 to fund its work training students and community members in NARCAN administration. Kevan Shah, the organization’s founder, was a rising sophomore at Muhlenberg College when he came up with the idea in 2019. He said the pandemic disrupted some of their plans, but they’ve had success holding virtual trainings over Zoom and mailing out NARCAN kits to trainees. To date, EOT has trained over 2,000 Pennsylvanians in NARCAN administration and certified 60 students as “peer educators” who can now lead their own training sessions.
 “Misconceptions about the use and misuse of opioids abound on college campuses,” Shah said. “It’s important for students to be trained in overdose recognition, prevention and NARCAN, not only during their years on campus but also for their experiences after campus.”
“Misconceptions about the use and misuse of opioids abound on college campuses,” Shah said. “It’s important for students to be trained in overdose recognition, prevention and NARCAN, not only during their years on campus but also for their experiences after campus.”
In states where the opioid crisis has hit hardest, colleges are taking extra measures. In 2019, West Virginia had the highest rate of opioid overdoses per capita of any state. An August 2019 survey of students at West Virginia University found that over half of the study sample reported receiving a prescription for opioids and almost 7 percent had witnessed an opioid overdose, yet only around 15 percent had received naloxone training.
The West Virginia Collegiate Recovery Network, housed at Marshall University in Huntington, is working to address this disparity. Founded in March 2020, the organization provides addiction support and overdose response training at West Virginia’s public institutions. Through its opioid response kit initiative, started this spring, WVCRN has provided 11 college campuses with “Naloxoboxes” and plans to bring them to 50 campuses across the state.
“We are fortunate to have support from many of our college and university presidents, and I’ve personally trained a number of them on how to use naloxone,” Susie Mullens, the network’s program coordinator, wrote in an email to Inside Higher Ed. “I am scheduled to train the new president of Marshall University later this week.”
Rising Urgency, Changing Attitudes
In February 2020, Eitan Weiner, a sophomore at Stanford University, overdosed in a fraternity house from what authorities say was a counterfeit Percocet containing lethal amounts of fentanyl.
Moss, the Stanford alumnus, was a junior at the time; he said the news was a wake-up call for the university community. He’d been an EMT and had seen firsthand the difference NARCAN could make between life and death. In the wake of Weiner’s overdose, Moss and a fellow student were inspired to push for NARCAN training and distribution across campus. They founded the Stanford Campus Opioid Overdose Prevention Project, or CO-OP, later that year.
“There was a massive shift in attitude at Stanford toward wanting NARCAN in as many hands as possible,” he said, adding that the initiative has received strong support from the university’s Office of Substance Use Programs, Education and Resources.
The Stanford case also highlights the liability concerns for universities when it comes to overdose risk. In January, Weiner’s family filed a wrongful death lawsuit against both the university and Weiner’s fraternity, Theta Delta Chi, which was disbanded in May 2021.
Vest, who also helps run the collegiate recovery program that coordinates much of Stanford’s naloxone training, is formerly incarcerated. He said his experience in the justice system taught him that a public health crisis deserves a public health response—and that reducing stigma around substance use is key to harm reduction.
“We are seeing a shift away from judgment and toward saving lives,” he said. “First and foremost, that’s what it’s all about.”





